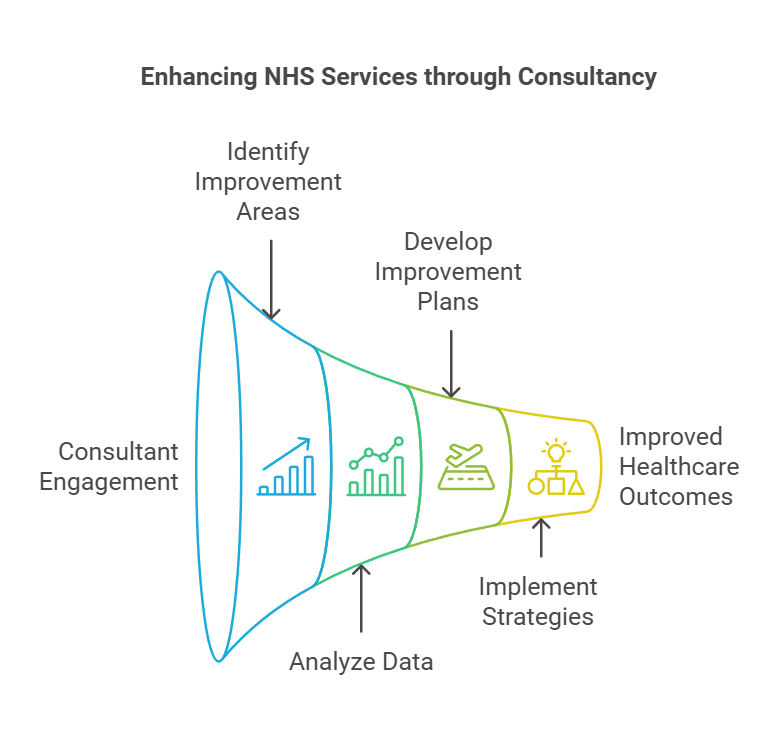
Healthcare Outcomes Improvement Consultants play a vital role in enhancing the quality and efficiency of NHS services. These professionals work closely with various NHS organisations to identify areas for improvement and implement effective strategies. Their expertise helps drive positive changes in patient care, operational processes, and overall healthcare outcomes.
The NHS relies on these consultants to bring fresh perspectives and innovative solutions to complex challenges. They analyse data, collaborate with staff at all levels, and develop tailored improvement plans. By fostering a culture of continuous improvement, these consultants contribute to the long-term sustainability and effectiveness of the NHS.
Working as a Healthcare Outcomes Improvement Consultant offers a unique opportunity to make a significant impact on the UK's healthcare system. It requires a blend of analytical skills, healthcare knowledge, and the ability to lead change in complex environments. Those in this role often find it rewarding to see their efforts translate into tangible improvements in patient care and NHS performance.
Key Takeaways
- Healthcare Outcomes Improvement Consultants drive positive changes in NHS services through strategic analysis and implementation
- These professionals require a diverse skill set, including healthcare expertise, data analysis, and change management abilities
- The role offers the opportunity to make a meaningful impact on patient care and NHS efficiency
Understanding The Healthcare Outcomes Improvement Consultant (NHS) Role
Healthcare Outcomes Improvement Consultants in the NHS play a vital role in enhancing patient care and system efficiency. They work across various levels of the health service, leveraging data and best practices to drive positive change.
Core Responsibilities In The Public Sector
Healthcare Outcomes Improvement Consultants focus on improving patient care and service delivery. They analyse data, identify areas for improvement, and develop strategies to enhance outcomes.
Key responsibilities include:
- Conducting audits and assessments of current practices
- Developing and implementing improvement initiatives
- Collaborating with NHS trusts, primary care, and integrated care boards
- Training staff on new processes and best practices
- Monitoring and evaluating the impact of interventions
These consultants often work across primary, secondary, and community care settings to ensure comprehensive improvements throughout the NHS.
Relevant Policy And Regulatory Context
Healthcare Outcomes Improvement Consultants must stay abreast of NHS policies and regulations. They work within the framework of NHS IMPACT, which supports continuous improvement across the health service.
Key policy areas include:
- Quality standards and patient safety guidelines
- NHS Long Term Plan objectives
- Care Quality Commission (CQC) regulations
- Data protection and information governance
Consultants must align their improvement strategies with these policies to ensure compliance and effectiveness. They also need to consider the broader context of healthcare provision, including the shift towards integrated care systems.
Typical Stakeholders And Decision-Making Processes
Healthcare Outcomes Improvement Consultants interact with a wide range of stakeholders across the NHS. They must navigate complex decision-making processes to implement changes effectively.
Key stakeholders include:
- NHS England leadership
- Clinical directors and senior management in NHS trusts
- Primary care network leads
- Integrated Care Board members
- Patient representatives and advocacy groups
Consultants often facilitate collaborative decision-making processes, bringing together diverse perspectives to agree on improvement priorities and strategies. They use evidence-based approaches to build consensus and drive change across different levels of the healthcare system.
Key Qualities and Areas of Expertise
Healthcare Outcomes Improvement Consultants in the NHS possess a unique blend of skills and knowledge. They combine technical expertise with institutional understanding and adaptable problem-solving abilities to drive positive change in patient care and health outcomes.
Technical/Subject-Matter Expertise
NHS consultants must have deep knowledge of quality improvement methodologies and evidence-based practices. They understand complex healthcare systems and can identify areas for enhancing patient safety and care quality.
These professionals are well-versed in data analysis and interpretation. They use this skill to measure outcomes and pinpoint unwarranted variations in care delivery.
Consultants also possess expertise in:
- Quality management systems
- Patient-centred care models
- Population health strategies
- Mental health best practices
Their knowledge spans both clinical and operational aspects of healthcare, enabling them to address multifaceted challenges effectively.
Institutional Knowledge and Networks
Successful consultants have a thorough grasp of NHS structures, policies, and procedures. They understand the organisation's priorities and can align improvement initiatives with overarching goals.
These professionals have built strong networks across various NHS departments and external partners. This allows them to:
- Facilitate collaboration between multidisciplinary teams
- Navigate complex organisational hierarchies
- Access and share best practices across the healthcare system
Their institutional knowledge helps them anticipate potential barriers to change and develop strategies to overcome them. They can effectively communicate with stakeholders at all levels, from frontline staff to senior management.
Adaptability and Problem-Solving Skills
Healthcare Outcomes Improvement Consultants must be agile thinkers capable of addressing diverse challenges. They can quickly analyse complex situations and develop innovative solutions tailored to specific contexts.
These professionals excel at:
- Identifying root causes of issues affecting patient outcomes
- Designing and implementing targeted interventions
- Adapting improvement strategies based on real-time feedback and results
They possess strong project management skills to oversee multiple initiatives simultaneously. Consultants can prioritise efforts that will have the most significant impact on reducing health inequalities and improving overall care quality.
Their problem-solving approach is collaborative, involving stakeholders at all levels to ensure buy-in and sustainable change.
Strategic Value to External Organisations
Healthcare Outcomes Improvement Consultants bring crucial expertise to external organisations working with the NHS. They offer insights into complex systems, policy trends, and data-driven approaches that can enhance service delivery and patient care.
Navigating Complex Procurement and Funding
NHS procurement processes can be challenging for external partners. Consultants help navigate these complexities, ensuring compliance with NHS standards. They guide organisations through:
• Tendering procedures
• Contract negotiations
• Funding applications
Consultants identify opportunities for innovation and research collaborations. Their expertise in NHS priorities aids in aligning proposals with current needs. This increases the chances of successful bids and partnerships.
Policy and Market Foresight
Consultants provide valuable insights into NHS policy directions and market trends. They help external organisations:
• Anticipate changes in healthcare delivery models
• Understand shifts in funding priorities
• Identify emerging technologies shaping the NHS
This foresight enables partners to develop products and services that meet future NHS needs. Consultants' knowledge of improvement science supports the creation of evidence-based solutions.
Enhancing Credibility and Compliance
External organisations benefit from consultants' deep understanding of NHS regulations and standards. This knowledge helps:
• Ensure products and services meet NHS requirements
• Align with NHS quality improvement initiatives
• Demonstrate value through robust evaluation methods
Consultants facilitate engagement with key NHS stakeholders, including local authorities and national improvement boards. This builds credibility and fosters collaborative relationships crucial for long-term success.
Leveraging Public Sector Data and Insights
Consultants offer unique access to NHS data and insights, valuable for external partners. They help organisations:
• Interpret complex healthcare data
• Identify areas for potential impact
• Develop targeted solutions based on real NHS needs
This data-driven approach supports innovation in areas such as artificial intelligence and digital health technologies. Consultants guide the ethical use of NHS data, ensuring compliance with governance frameworks.
Practical Outcomes and Applications
Healthcare Outcomes Improvement Consultants in the NHS focus on tangible results and real-world applications. Their work drives positive change in patient care, service delivery, and overall health system performance.
Product Development and Service Enhancement
Consultants play a key role in developing new healthcare products and services. They analyse current offerings and identify gaps in patient care. This process often involves:
• Conducting clinical audits
• Gathering feedback from service users
• Reviewing electronic patient records
Through these methods, consultants pinpoint areas for improvement. They then work with clinical teams to design and implement enhanced services.
Co-production is a vital part of this process. Consultants involve patients and staff in developing new care pathways. This approach ensures services meet real needs and are user-friendly.
Go-To-Market and Engagement Strategies
Once new products or services are ready, consultants help with rollout plans. They create strategies to engage both staff and patients. This might include:
• Training programmes for healthcare professionals
• Information campaigns for patients
• Digital tools to support service adoption
Consultants also work on improving patient care together through NHS IMPACT. This initiative aims to spread best practices across the health system.
Long-Term Sustainability and Growth
Ensuring long-term success is crucial. Consultants develop strategies for ongoing improvement and expansion of services. They might:
• Set up continuous feedback loops
• Establish regular review processes
• Create scalable models for successful initiatives
Consultants also focus on workforce development. They help create training programmes to build staff skills and knowledge. This supports the growth and sustainability of new services.
Measuring Impact and ROI
Tracking outcomes is essential to prove the value of new initiatives. Consultants set up systems to measure:
• Patient outcomes
• Service efficiency
• Cost-effectiveness
They use data from clinical outcomes reporting to show the impact of changes. This might include improvements in waiting times, patient satisfaction, or health outcomes.
ROI calculations help justify investment in new services. Consultants present clear evidence of benefits to support future funding decisions.
Frequently Asked Questions
NHS service improvement involves enhancing healthcare outcomes through various initiatives and projects. Consultants play a key role in guiding these efforts to boost quality and efficiency.
What are some notable examples of service improvement within the NHS?
The NHS has implemented several successful service improvements. One example is the National Clinical Improvement Programme, which provides surgeons with online access to their patient outcomes data. This helps identify areas for improvement in surgical practices.
Another notable initiative is the development of Strategic Clinical Networks. These networks foster collaboration among healthcare professionals to enhance quality of care in specific areas like cancer and mental health.
How can healthcare outcomes be enhanced through NHS service improvements?
NHS service improvements can boost healthcare outcomes in multiple ways. One approach is using clinical outcomes data to drive changes. Analysing patient outcomes helps identify areas needing improvement and measure the impact of interventions.
Implementing evidence-based practices and standardising care pathways can also lead to better outcomes. Regular audits and feedback loops ensure continuous improvement in patient care quality.
What is the significance of service improvement within healthcare settings?
Service improvement in healthcare is crucial for several reasons. It helps optimise resource use, reducing waste and improving efficiency. This is especially important given limited NHS budgets.
Improved services lead to better patient experiences and outcomes. This can increase patient satisfaction and trust in the healthcare system. Service improvements also boost staff morale by streamlining processes and reducing frustrations.
Can you describe the functions of the healthcare outcomes improvement consultant within the NHS?
Healthcare outcomes improvement consultants in the NHS have several key functions. They analyse data to identify areas for improvement in patient care and outcomes. This involves reviewing clinical data, patient feedback, and performance metrics.
Consultants also work with clinical teams to develop and implement improvement strategies. They may provide training on quality improvement methods and tools. Additionally, they often help measure and report on the impact of improvement initiatives.
What constitutes a Quality Improvement Project (QIP) within the NHS framework?
A Quality Improvement Project (QIP) in the NHS aims to enhance a specific aspect of healthcare delivery. It typically follows a structured approach, such as the Plan-Do-Study-Act (PDSA) cycle.
QIPs often focus on areas like reducing waiting times, improving patient safety, or enhancing clinical outcomes. They involve setting clear goals, collecting and analysing data, and implementing targeted interventions.
What has NHS Improvement been rebranded to and what implications does this have for service enhancement?
NHS Improvement merged with NHS England in April 2019. This new combined organisation is now simply called NHS England. The merger aims to provide more joined-up support for the health service.
This change allows for better coordination of improvement efforts across the NHS. It helps align national priorities with local implementation, potentially leading to more effective service enhancements.