The UK government provides valuable data for analysing healthcare procurement practices. This information helps NHS organisations improve their purchasing strategies and save money. The NHS Procurement Dashboard offers a balanced scorecard of core metrics focused on business continuity, efficiency, and risk mitigation.
NHS trusts can use this data to compare their performance with others and identify areas for improvement. The NHS Spend Comparison Service is an online tool that allows procurement teams to compare price and spend data. This helps them find potential savings and work together to purchase goods and services more effectively.
By using gov.uk data, healthcare organisations can make better decisions about their procurement practices. This can lead to cost savings, improved efficiency, and better patient care. The data provides insights that can drive innovation and modernisation in the NHS.
Key Takeaways
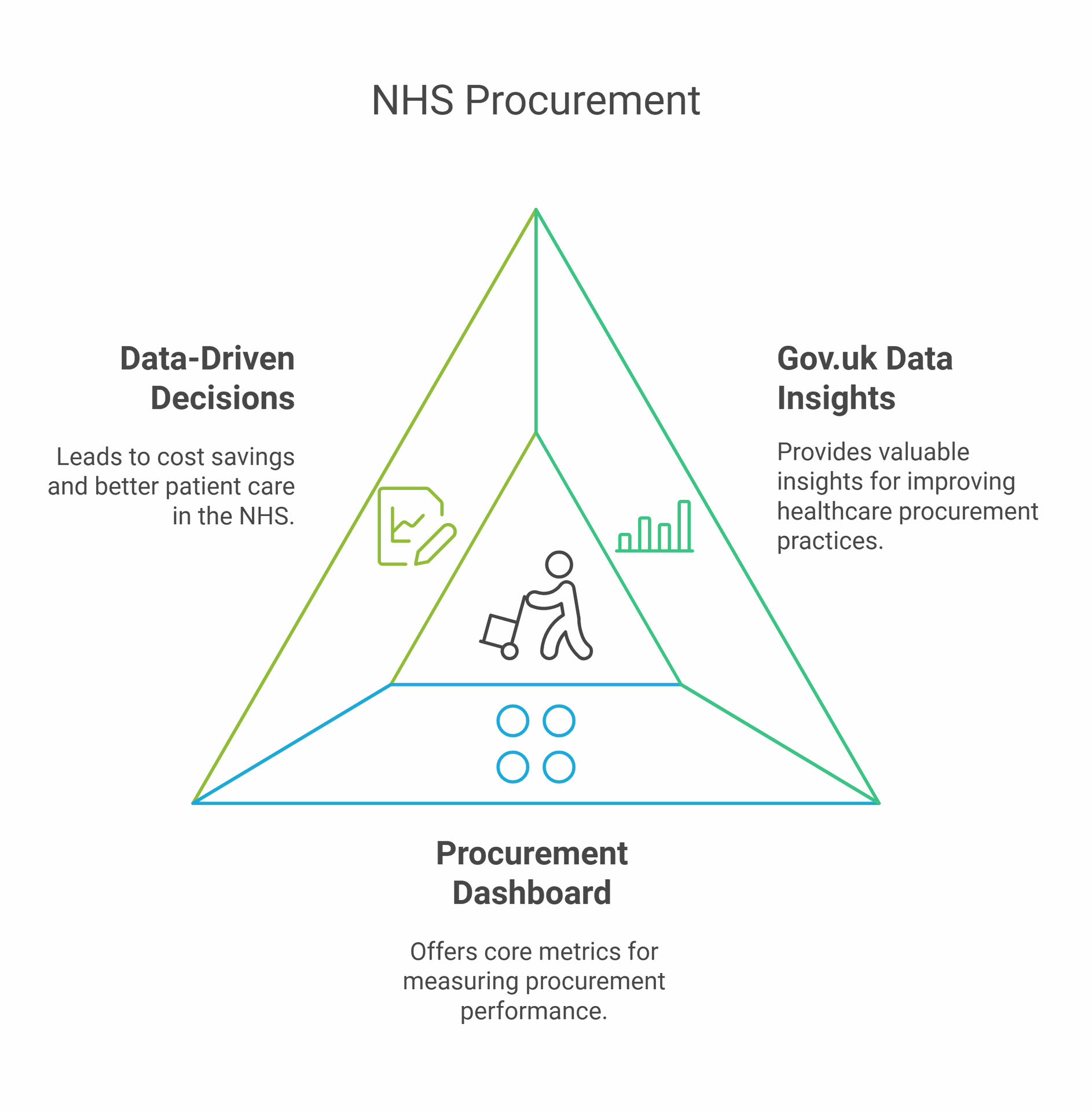
- Gov.uk data offers valuable insights for improving healthcare procurement practices
- The NHS Procurement Dashboard provides core metrics for measuring procurement performance
- Data-driven decision making can lead to cost savings and better patient care in the NHS
Understanding Healthcare Procurement in the UK
The NHS and Department of Health and Social Care play crucial roles in healthcare procurement. Current processes face challenges, but data analysis offers opportunities for improvement. Effective procurement impacts patient care and NHS efficiency.
The Role of NHS and DHSC
The National Health Service (NHS) is the UK's largest purchaser of goods and services. It spends over £27 billion annually on procurement. The Department of Health and Social Care (DHSC) sets procurement policy and strategy.
The NHS works to get value for money in its purchasing. This helps stretch limited budgets further. The DHSC aims to improve NHS procurement practices. It does this through guidance and mandates.
NHS trusts handle most day-to-day purchasing decisions. They buy medical supplies, equipment, and services. The goal is to meet local needs efficiently.
Current Procurement Processes and Challenges
NHS procurement involves complex processes. These include needs assessment, tendering, and contract management. Trusts must follow public sector purchasing rules.
Challenges include:
• Fragmented purchasing across trusts
• Lack of spending data visibility
• Varying levels of procurement expertise
• Difficulty comparing prices between suppliers
The NHS has worked to address these issues. It has introduced e-procurement systems to streamline processes. These aim to reduce paperwork and errors.
Centralised frameworks now exist for some common goods. This helps leverage the NHS's buying power. But local variation in needs still presents challenges.
Importance of Data in Healthcare Procurement
Data plays a vital role in improving NHS procurement. It helps identify savings opportunities and benchmark performance. The NHS has developed tools to harness procurement data.
The NHS Procurement Dashboard is one such tool. It provides metrics for trusts to measure their performance. This increases transparency and drives improvement.
Good data supports:
• Price comparisons between suppliers
• Spend analysis to spot inefficiencies
• Forecasting of future needs
• Evidence-based decision making
Better use of data can lead to significant savings. This frees up resources for patient care. It also helps ensure the NHS gets the best value from its spending.
Data Sources and Accessibility
The UK healthcare system relies on various data sources for procurement analysis. These sources offer valuable insights into population health, healthcare utilisation, and service delivery patterns.
ONS Statistics and Public Health Data
The Office for National Statistics (ONS) provides crucial population and health data for healthcare procurement analysis. ONS conducts the national census every 10 years, offering detailed demographic information.
Key ONS datasets include:
- Population estimates
- Birth and death rates
- Life expectancy figures
- Health inequality statistics
Public Health England (now part of the UK Health Security Agency) publishes data on:
- Disease prevalence
- Health behaviours
- Environmental health factors
These datasets help identify healthcare needs and inform resource allocation decisions.
General Practice Extraction Service (GPES)
GPES is a vital source of primary care data. It extracts information from GP practices across England, providing insights into:
- Patient diagnoses
- Prescribing patterns
- Referrals to secondary care
This data is crucial for understanding primary care demand and planning procurement strategies. GPES data helps identify trends in chronic disease management and preventive care needs.
Healthcare analysts use GPES data to:
- Forecast medication requirements
- Plan specialist services
- Evaluate the effectiveness of public health interventions
Hospital Episode Statistics and NHS Data
Hospital Episode Statistics (HES) offer a comprehensive view of secondary care utilisation in England. This dataset includes:
- Inpatient admissions
- Outpatient appointments
- A&E attendances
HES data provides valuable insights into:
- Procedure volumes
- Length of stay
- Readmission rates
NHS Digital (now part of NHS England) manages various other datasets, including:
- Workforce statistics
- Patient experience surveys
- Waiting times data
These sources help procurement teams understand service demands, identify efficiency opportunities, and plan for future healthcare needs.
Data Analysis for Strategic Procurement
Data analysis plays a key role in healthcare procurement. It helps NHS trusts make smart choices about supplies and save money. Let's look at how data shapes procurement decisions, real-world examples, and ways to invest wisely.
Interpreting Data for Procurement Decisions
NHS trusts use data to guide their buying choices. They look at past spending patterns to spot trends. This helps them predict future needs.
Trusts also compare their data with other healthcare providers. This process is called benchmarking. It shows where they can cut costs or get better deals.
Some key data points trusts analyse:
- Supplier performance
- Stock levels
- Delivery times
- Product quality
- Price trends
By studying these factors, trusts can pick the best suppliers and products. They can also time their purchases to get the best value.
Case Studies: NHS Trusts and Procurement Efficacy
Real examples show how data analysis improves procurement.
One trust used data to spot overspending on gloves. They switched suppliers and saved £100,000 a year.
Another trust analysed their stock data. They found they were ordering too much of some items. By fixing this, they freed up storage space and cut waste.
A group of trusts shared their procurement data. This helped them negotiate better deals with suppliers. They saved millions on common items like bandages and syringes.
These cases prove that data-driven decisions lead to smarter spending and better patient care.
Investment and Savings Opportunities
Data analysis reveals where trusts can invest to save money long-term.
One area is technology. Trusts can invest in better data systems. These help track spending and stock levels more accurately.
Another opportunity is staff training. Trusts can invest in courses to help procurement teams understand data better. This leads to smarter buying choices.
Bulk buying is another way to save. Data shows which items are used most. Trusts can then buy these in large amounts for discounts.
Some trusts invest in sustainable products. Data shows these often cost less over time, despite higher upfront costs.
By using data wisely, NHS trusts can find the right balance between spending and saving. This ensures they have the supplies they need while keeping costs down.
Legal and Ethical Considerations
Using health data for procurement analysis comes with important legal and ethical duties. Protecting patient privacy and keeping data secure are top priorities.
Data Protection and Patient Consent
The Data Ethics Framework guides public sector data use in the UK. It stresses safeguarding patient information.
Health data is sensitive. Analysts must follow strict rules. The law requires getting patient consent in many cases.
When consent isn't needed, data should be anonymised. This means removing names and other details that could identify people.
Procurement teams should work with data experts. They can help make sure analysis follows the rules. Breaking data laws can lead to big fines.
Security Measures for Health Data
Health data needs strong protection. The NHS and other groups use many safety steps.
Encryption is key. This scrambles data so only approved people can read it. Secure networks also help keep data safe as it moves around.
Access controls are vital. Only staff who need the data should be able to see it. Logs track who looks at data and when.
Regular security checks help spot weak points. Teams should test their defences often. They must also have plans ready in case of data breaches.
Staff training is crucial. Everyone who handles health data needs to know the risks and rules.
Collaboration and Stakeholder Engagement
Effective healthcare procurement analysis relies on strong partnerships and clear communication across sectors. Bringing together diverse perspectives helps drive innovation and ensure data-driven decisions benefit patients and the public.
Role of Research Funders and Academia
Research funders and academic institutions play a vital role in advancing healthcare procurement practices. They provide crucial funding and expertise to analyse large datasets and identify trends.
Universities often partner with NHS trusts to conduct in-depth studies on procurement efficiency. This collaboration helps develop new analytical tools and methodologies.
Research councils fund projects exploring innovative ways to use procurement data. These initiatives aim to improve patient outcomes whilst optimising resource allocation.
Academia also offers training programmes for NHS procurement staff. These courses enhance analytical skills and promote evidence-based decision making.
Patient Representatives and Public Communication
Including patient voices in procurement analysis ensures decisions align with public needs. Patient representatives provide valuable insights into the real-world impact of purchasing choices.
NHS trusts often establish patient advisory groups to review procurement data. These groups help identify areas where spending can better address patient priorities.
Clear public communication about procurement analysis builds trust. NHS organisations use websites and social media to share key findings and explain how data informs decisions.
Infographics and simple summaries make complex procurement data accessible to the public. This transparency helps demonstrate responsible use of public funds.
Interoperability with IT Systems and Transformation Projects
Seamless integration of procurement data with existing NHS IT systems is crucial. This interoperability allows for more comprehensive analysis and informed decision-making.
Many NHS trusts are implementing new data sharing protocols to support procurement analysis. These efforts aim to break down data silos and create a more holistic view of spending patterns.
Transformation projects often focus on upgrading procurement software. Modern systems offer advanced analytics capabilities, helping staff identify cost-saving opportunities.
Integration with electronic patient records systems allows procurement teams to link spending directly to patient outcomes. This data-driven approach supports more effective resource allocation.
Innovation and Modernisation Through Data
The UK government is using data to drive major changes in healthcare. New tools and systems are making the NHS work better. These efforts aim to improve patient care and make operations more efficient.
Leveraging Data for NHS Modernisation
The NHS is using data to transform services. This includes giving patients more access to their health records through the NHS App. Patients can now see their GP records and have more control over how their data is used.
The NHS is also making it easier for researchers to access health data safely. This helps drive medical breakthroughs and improve treatments. The goal is to use data to make healthcare better and more personalised for each patient.
Key areas of focus include:
- Improving data security and privacy
- Making data more accessible to researchers
- Using data to redesign services
Development of a Minimum Viable Product (MVP)
The NHS is taking a step-by-step approach to data projects. They often start with a minimum viable product. This means creating a basic version of a new system or tool quickly. They then test and improve it over time.
This approach helps the NHS:
- Get new ideas up and running faster
- Test concepts with real users
- Make changes based on feedback
One example is the NHS App. It started with basic features and has grown to include more services over time. This method helps the NHS innovate while managing risks and costs.
Data Architecture and Engineering in Healthcare
The NHS is building new data systems to support modern healthcare. This involves creating a strong data architecture. It's about organising data so it's easy to use and secure.
Key parts of this work include:
- Setting up secure data environments for research
- Creating standards for how data is stored and shared
- Building systems that can handle large amounts of health data
Engineers are working to make sure different NHS systems can talk to each other. This helps doctors and nurses get the information they need quickly. It also supports better planning and decision-making across the healthcare system.
Methodological Approach
The methodological approach for using gov.uk data in healthcare procurement analysis involves systematic data collection, thorough desk research, and careful interpretation. These methods ensure reliable insights for decision-making.
Data Collection Techniques
Gov.uk data serves as a primary source for healthcare procurement analysis. Researchers use automated scraping tools to gather relevant information from the website.
They focus on procurement notices, contract awards, and spending data. This data is often available in machine-readable formats like CSV or JSON.
Analysts also collect supplementary data from NHS trusts and clinical commissioning groups. They may use surveys or direct requests to obtain specific procurement details not available on gov.uk.
Desk Research and Interviews
Desk research involves examining existing reports, academic papers, and policy documents. Analysts review past procurement trends, best practices, and regulatory changes.
They analyse NHS Procurement & Commercial Standards to understand current guidelines. This helps identify areas for improvement in procurement processes.
Interviews with procurement professionals provide valuable context. Researchers conduct structured interviews with NHS buyers, suppliers, and policymakers. These discussions offer insights into practical challenges and successful strategies.
Data Interpretation and Reporting
Analysts use statistical software to process and interpret the collected data. They perform trend analysis, cost comparisons, and supplier performance evaluations.
Visualisation tools help create clear, informative graphs and charts. These visuals make complex procurement data more accessible to stakeholders.
Reports typically include:
- Executive summary
- Methodology overview
- Key findings and trends
- Recommendations for improving procurement practices
Researchers ensure their reports are written in plain language. They focus on actionable insights that can drive efficiency and cost-savings in NHS procurement.
Challenges and Recommendations
The NHS faces several hurdles in using data for healthcare procurement analysis. These include technical complexities, data sharing issues, and the need to improve patient outcomes through better access to information. Strategic planning is key to overcoming these obstacles.
Navigating Technical Aspects and Data Sharing
NHS trusts struggle with complex procurement data. Many lack the skills to analyse this information effectively. Data sharing between trusts is often limited, making it hard to compare practices.
Trusts need better tools to make sense of procurement data. Training staff in data analysis could help. A central system for sharing anonymised data might allow trusts to learn from each other.
Security concerns sometimes limit data sharing. Clear guidelines on data protection could ease these worries. Encouraging a culture of openness while respecting privacy is crucial.
Promoting Data Access and Patient Outcomes
Limited access to health data hinders research and improvement efforts. Better data access could lead to more efficient procurement and better patient care.
Recommendations:
- Create user-friendly platforms for researchers to access health data
- Develop clear processes for data requests
- Ensure data is high-quality and up-to-date
Linking procurement data to patient outcomes is vital. This could show which supplies lead to better results. It might also highlight areas where spending could be more effective.
Strategic Recommendations for Service Planning
Strategic planning is key to improving NHS procurement. Data-driven decisions can lead to better service delivery and cost savings.
Key steps:
- Implement Reproducible Analytical Pipelines (RAP) across the NHS
- Use benchmarking to identify best practices
- Encourage trusts to share successful procurement strategies
Regular reviews of procurement data can help spot trends and issues early. This allows for quick adjustments to service planning.
Involving clinicians in procurement decisions is crucial. Their insight can ensure that cost-saving measures don't compromise care quality.
Impact of Data on the Future Healthcare Landscape
Data is reshaping the UK healthcare system. It's driving innovation, improving patient care, and transforming how the NHS operates. The effects are far-reaching, from pandemic response to long-term strategic planning.
Evaluating the Impact of COVID-19 on Data Usage
The COVID-19 pandemic sparked a data revolution in healthcare. The NHS rapidly adopted new ways to collect and analyse patient information. This led to faster decision-making and more targeted interventions.
Data-driven healthcare became crucial for tracking virus spread and vaccine effectiveness. The NHS used real-time data to manage hospital capacity and allocate resources efficiently.
The pandemic also highlighted the need for better data sharing between different parts of the health system. This spurred efforts to create more integrated data systems across the NHS.
Health and Care System Transformation
Data is driving a major shift in how the NHS delivers care. It's enabling more personalised treatments and preventive care strategies.
Advanced data analysis is helping to identify high-risk patients earlier. This allows for timely interventions that can prevent serious health issues.
The NHS is using data to streamline operations and reduce waiting times. Predictive models help forecast demand for services, allowing for better resource allocation.
Digital health technologies, powered by patient data, are expanding access to care. Telemedicine and remote monitoring are becoming more common, especially in rural areas.
Influence of Patient Data Research on NHS Practices
Patient data is fuelling medical research and driving evidence-based practices in the NHS. Large-scale studies using anonymised patient records are uncovering new insights into diseases and treatments.
The NHS Data Saves Lives initiative is promoting the responsible use of patient data for research. This is leading to faster development of new drugs and therapies.
Genomic research, powered by patient data, is enabling more precise diagnoses and treatments. The NHS is increasingly using genetic information to tailor care to individual patients.
Patient data is also helping to identify and address health inequalities. Research is revealing disparities in care access and outcomes, informing policy changes to improve healthcare equity.
Frequently Asked Questions
The NHS utilises data-driven approaches to enhance healthcare procurement efficiency and improve public health outcomes. Key aspects include strategic frameworks, eProcurement initiatives, and data analysis for informed decision-making.
How is healthcare procurement data utilised within the NHS?
The NHS uses procurement data to benchmark expenditure against other trusts and healthcare providers. This comparison helps identify areas for cost savings and efficiency improvements.
Data analysis also supports population health planning. The NHS Federated Data Platform enables access to relevant information for direct care and strategic planning purposes.
What are the components of the NHS procurement framework?
The NHS procurement framework includes several key elements. These comprise standards of procurement arranged under four domains: leadership, process, partnerships, and people.
The framework also emphasises the importance of qualified procurement staff. It tracks the percentage of recognised procurement staff with appropriate formal qualifications.
How does the NHS eProcurement strategy enhance supply chain efficiency?
The NHS eProcurement strategy focuses on automating data exchange and adopting master procurement data. It mandates the use of GS1 and PEPPOL standards to improve consistency and interoperability.
This approach aims to streamline processes, reduce errors, and increase transparency throughout the supply chain.
What is the origin and impact of the 'Data Saves Lives' initiative?
The 'Data Saves Lives' initiative emphasises the importance of data in improving healthcare outcomes. It promotes responsible data use for research, planning, and service improvement.
The initiative supports better decision-making in healthcare by ensuring that relevant, high-quality data is available to those who need it.
Why is data analysis crucial for the improvement of public health responses?
Data analysis enables the NHS to identify trends, predict future needs, and allocate resources effectively. It helps in understanding population health patterns and planning targeted interventions.
By analysing procurement data, the NHS can ensure that supplies and services are available where and when they are most needed, improving overall public health responses.
In what ways can NHS procurement contracts be accessed and analysed for healthcare improvement?
NHS procurement contracts can be accessed through various platforms, including the Provider Selection Regime. This regime applies to the procurement of healthcare and public health services.
Analysis of these contracts can reveal spending patterns, supplier performance, and potential areas for improvement in service delivery and cost-effectiveness.